The measles…years after your child gets sick.
Here in America, as in many countries around the world, we are seeing large outbreaks of the measles due to falling vaccine rates. It’s all over the news—what measles looks like, how contagious it is, what it can do the body, and most importantly, how it can be prevented: vaccination.
However, there are things you aren’t hearing about the measles. Frightening things.
You may have heard that there are complications that may arise after contracting the measles virus such as ear infections, diarrhea, pneumonia, encephalitis (that can lead to deafness/intellectual disability), and death.
These complications are more common in small children with immature immune systems under 5 and adults over 20 with immune system compromise.(5)
But what can happen to these children and adults years after overcoming the measles?
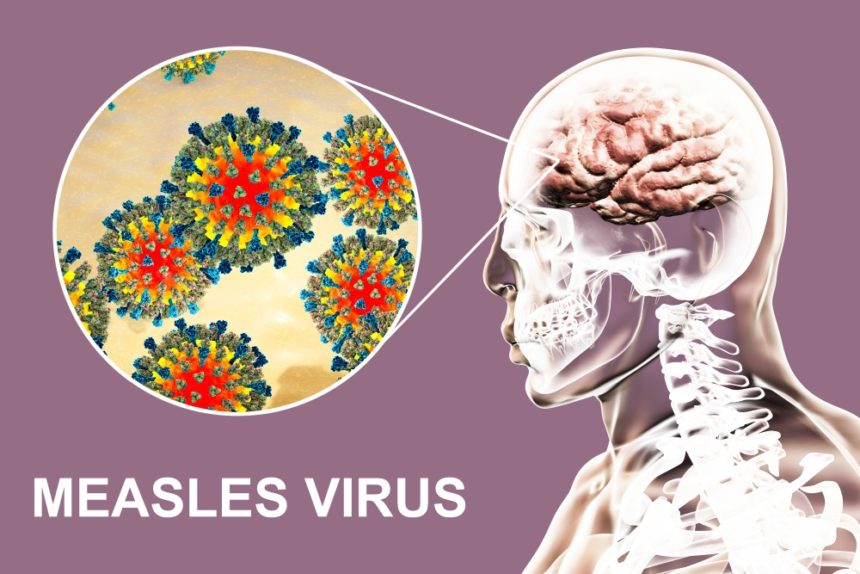
Data shows that around 4-11 people out of 10,000 will get a rare but fatal disease called subacute sclerosis panencephalitis (SSPE).
This disease leads to swelling and inflammation in the brain. Subacute sclerosis panencephalitis is progressive, disabling, and fatal. Almost all people pass away 1-3 years after diagnosis.
Since SSPE is slowly progressing, a measles survivor seems to be otherwise healthy. However, around 7-10 years [with a range from 1 month to 27 years (1)] after contracting the measles, SSPE victims will rear its ugly face.
That means a child who contracted the measles before the age of two most likely would show symptoms of the disease around their tenth birthday.
Studies suggest that children who contracted the measles at under two years of age are more likely than older children and adults to develop SSPE, with a 3 times higher risk to males.
Some of the diagnostic signs of SSPE are damage to the optic nerve/retina, muscle twitching, and poor motor coordination.
This disease is progressive and comes in stages:
- Stage One: This begins with a fever and headache and coincides with personality changes, mood swings, and/or depression. These symptoms may last up to six months.
- Stage Two: The patient progresses with uncontrolled movements such as jerking and muscle spasms. They may develop dementia, seizures, and blindness.
- Stage Three: The jerking movements become twisting movements and the body may go rigid. Complications from this could lead to death.
- Stage Four: Damage to the areas of the brain that control breathing, heart rate, and blood pressure leads to a vegetative state and eventually death.
There is no cure for SSPE. Doctors may be able to control the symptoms and boost the immune system for some time before the disease fully overcomes the individual. Current findings report 95% of patients will succumb to the disease.(5)
With SSPE victims, the understanding is that it’s caused by an abnormal immune response to the virus most likely caused by an immature immune system/central nervous system.(3) However, some scientists suggest it may be caused by a mutant form of the virus. This theory is growing steam.
The disease is untreatable, but it is 97% preventable with the very effective measles vaccine. The vaccine will not cause disease and it’s track record with preventing SSPE is tremendous.
More often than not, the measles virus will not cause SSPE brain damage. Subacute sclerosis panencephalitis is very rare, however, do you want to gamble with your child’s life?
If this isn’t enough to go grab your unvaccinated child an MMR vaccine, then head on over and read these new findings on the measles virus and the destruction of the immune system. <– a MUST read.
Please consider all of the consequences when deciding to skip the vaccine. The MMR vaccine safe and effective and most importantly, saves lives.
Some other measles-related articles that may be of interest:
Measles Kills. Vaccines Save Lives!
References:
- Schönberger, K., Ludwig, M. S., Wildner, M., & Weissbrich, B. (2013). Epidemiology of subacute sclerosing panencephalitis (SSPE) in Germany from 2003 to 2009: a risk estimation. PloS one, 8(7), e68909. doi:10.1371/journal.pone.0068909
- MedlinePlus. “Subacute sclerosing panencephalitis.”
- Miller C, Farrington CP, Harbert KInt J Epidemiol. The epidemiology of subacute sclerosing panencephalitis in England and Wales. 1970-1989. 1992 Oct; 21(5):998-1006.
- Pallivathucal LB, Noymer A. Subacute sclerosing panencephalitis mortality, United States, 1979-2016: Vaccine-induced declines in SSPE deaths. Vaccine. 2018;36:5222-5225
- Jafri, S. K., Kumar, R., & Ibrahim, S. H. (2018). Subacute sclerosing panencephalitis – current perspectives. Pediatric health, medicine and therapeutics, 9, 67–71. doi:10.2147/PHMT.S126293
- National Institute of Neurological Disorders and Stroke (NINDS). “Subacute Sclerosing Panencephalitis“